Today’s Heart Disease Survivors Aren’t Who You Think They Are

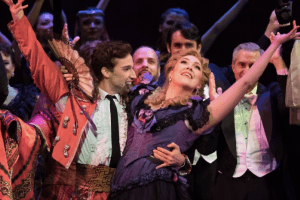
Photo credit: Nell Hoving
More than 350,000 people die of heart disease in the U.S. each year, but there’s one image that usually comes to mind as the typical heart attack patient: an older, overweight man.
With tens of thousands of victims each year who don’t fit that mold, the stereotype is a problem. Since 1979, the death rate for heart disease in men has declined steadily by 21.5 percent, while the death rate for women has declined by only 9.9 percent, according to the American Heart Association. Women are also more likely than men to die within a year of having an initial heart attack, partly because they’re less likely than men to receive certain diagnostic testing and treatments.
As demographics shift, it’s vital that research and education follow. That means ensuring that gender-specific information about symptoms, risk factors and new medical treatments is available to medical professionals and the public.
A new wave of survivors of all stripes are stepping up to share their stories and raise awareness about the fact that heart disease can impact everyone—even those who life an extremely healthy life—especially if they have a family history of heart problems or have other risk factors, such as being post-partum.
We spoke with five of those survivors about their stories and activism. While their experiences were unique, there was one thread that connected them all: They never thought it would happen to them.
Stephanie Austin, 46

Photo credit: Nell Hoving
Heart disease survivor since 2008
Ten years ago, a typical evening for Stephanie Austin involved a soccer match that stretched past midnight, followed by drinks with her teammates, and then a 6 a.m. wake-up with her kids. At 35, she was in the best shape of her life—juggling a slew of athletics (tennis, three co-ed soccer teams, regular trips to the gym to lift weights) with being an active mom to her two boys, Alec and James , even serving as PTA president at the preschool.
“I was very type A,” Austin says. “And sports were kind of my thing—they always identified me. I’d joke that ‘Oh, I’m not the prettiest; I’m not the wealthiest; I’m not the smartest; but I’ll kick all your asses.’”
That all changed one night when Stephanie’s husband, Matt, an orthopedic surgeon, was awakened by an early morning call. While on the phone, he noticed Stephanie’s breathing was irregular and she was non-responsive. He called 911 and performed CPR until help arrived. When she awoke the next day, her speech was slurred and she didn’t recognize her family. The doctors didn’t know if she would come back from the brain damage caused by cardiac arrest.
“The kids couldn’t come see me for a couple days because I didn’t know who they were,” Austin remembers. “My cousin brought a picture of the boys, and I said ‘Oh they’re cute, who are they?’”
Austin ended up leaving the hospital two weeks later with a pacemaker and defibrillator in her chest. She never regained her memories from the year preceding or following the accident. She still describes her short-term memory as “horrendous,” and she has a lot of limitations on how high she can raise her heart rate.
While Austin went overnight from being able to play a 90-minute soccer game to not being able walk around the block, she feels extremely lucky. The survival rate for sudden cardiac arrest that happens outside of a hospital is less than 10 percent, and of that 10 percent, the percentage that resumes a fairly normal life is quite small. While she’s not as active on the field as she once was, she’s found a new arena to stay busy.
“Working with the AHA for the past six years has allowed me to use my voice to raise awareness and funds, which has been a real blessing,” Austin says. She’s been on the board for the Philly branch of six years, advocates in Harrisburg for CPR training in schools and citywide, hosts “CPR Parties” at her home where her community can become certified, and speaks regularly on heart disease. “When you hear a person’s story and you see their face, there’s so much power that comes from that. And from that power comes action. That’s really what we needed—Not just increased awareness, but action.”
Zelma Brantley, 67

Photo credit: Nell Hoving
Heart disease survivor since 2015
Zelma Brantley was in her first year of retirement and enjoying life when she mentioned to her doctor at her annual checkup that she was experiencing some indigestion but “nothing serious.”
“Thank God he took it a step further and did a stress test,” Brantley says. The test showed a blockage, which led to more testing, which showed a fully blocked artery. Armstrong was admitted to the hospital immediately, and heart surgery was scheduled for the following week.
“I was hysterical,” Brantley says. “I would have never thought in a million years this would happen to me. You hear about people having problems with their heart, but I never had those symptoms and I’m the type of person that takes care of herself.”
Brantley ended up having robotic heart surgery and then entering cardiac rehab. She says recovery and heart health is now a lifelong process, and she goes to the gym in her River Park neighborhood 2-3 times a week to exercise to keep her arteries open. While she’s feeling healthy and doesn’t have shortness of breath, she’s now balancing caring for her husband while caring for herself.
“My husband is sick right now—he has stage four lung cancer—so I’m dealing with that and trying to keep doing what I need to do to stay healthy,” she says.
Today, Brantley stresses the important of listening to one’s body.
“You know your body and you know when something isn’t normal,” she says. “Even if you think it’s nothing serious, at least get it checked out.”
Amy Cavaliere, 37

Photo credit: Nell Hoving
Heart disease survivor since 2017
There are a lot of reasons, Amy Cavaliere says, that she shouldn’t be here. Her husband was supposed to be out of town for work the morning she began experiencing symptoms, but he had decided to come home for their kids’ open house. She told him she must just be having her first panic attack, but he didn’t listen and called an ambulance, which was where she went into cardiac arrest and lost consciousness. Typically, paramedics wouldn’t keep up CPR for more than 40 minutes, but they were extraordinarily persistent.
And most people wouldn’t wake up from what happened next—a fully occluded coronary artery resulted from SCAD (Spontaneous Coronary Artery Dissecation); seizures; an 8-day, medially-induced coma and life support; double pneumonia which lead to severe tracheal stenosis; and an emergency bronchosocopy. But, somehow, Cavaliere did.
“The hospital staff had done everything they could do, and asked my family to prepare for the worst, but never gave up on me,” Cavaliere says. “While in the throes of the pneumonia, a pulmonologist at the hospital decided to try one last medication to improve my lung function, and it essentially brought me back to life. I survived.”
Cavaliere is in the middle of cardiac rehabilitation to strengthen her heart, and still takes multiple medications every day. She gets easily winded chasing after her kids or even pushing a grocery cart, and doctors say it could take up to two years to feel fully like herself. But for Cavaliere, feeling like herself is no small thing. As someone who nearly didn’t survive on so many occasions, she says she now feels a constant drive to share her story to help others see the warning signs or show other survivors that they’re not alone.
“The face of cardiac arrest isn’t just someone old or physically out of shape. It’s me, and plenty of other young people and mothers who do everything right to maintain their health,” Cavaliere says. “It shouldn’t have happened to me, but it did. And I’m committed to helping others get through it, just as I have done.”
Andrea Cardwell, 41

Photo credit: Nell Hoving
Heart disease survivor since 2017
Andrea Cardwell’s health journey started long before heart disease. At the age of 22, and then again at 32, Cardwell fought off a rare bone cancer called Ewing’s Sarcoma. After going into remission for the second time, Caldwell found herself ready to take on the next challenge: motherhood. Unfortunately, her pregnancy was also not without difficulties.
“Around 20 weeks into my pregnancy, I was having a lot of shortness of breath and swelling in my ankles and feet and I couldn’t sleep lying down,” says Cardwell, an ICU nurse. Cardwell told doctors she felt like a patient with congestive heart failure, but for months her symptoms were disregarded and labeled as “normal” for someone carrying twins.
“I wanted a normal pregnancy so I trusted them, but in the back of my head I knew something was wrong,” she says.
When she gave birth via C-section at 30 weeks, she was sent home again, despite ongoing wheezing and swelling. When she returned to the hospital a few days later because she could barely breath (her husband, Tom, says she sounded “like she was speaking underwater”), they gave her antibiotics for bronchitis and tried to send her home again. At that point, she put her foot down and refused to leave until they performed an echocardiogram, which revealed that her heart was functioning at only 20 percent.
Once Cardwell was properly treated for heart failure, she lost 50 pounds of fluid that her kidneys weren’t properly pumping out. She also received an external defibrillator vest with a battery pack that she had to wear for five months—even as she cared for her two infants, recovered from a C-section, and went back to work as a nurse several months later. Her heart resumed normal function within the year, so for now she doesn’t need to pursue normal treatment. Recovery has come with its own challenges, though. She’s still slowly getting back into a rhythm where she can exercise and run around with her healthy toddlers, Allison and Vincent.
“Last time around this year, I just got depressed thinking ‘why me?’” she says. “But I just pushed through it, like every other time. You have to. You don’t have a choice. I have so much to live for and life is so short.”
She also shares her story to encourage other women to be as unceasingly persistent as she was when they know something is wrong—even if they’re being made to feel crazy.
“Keep going until you find somebody to hear you,” Caldwell says. “Be your own advocate. Don’t rely just on the medical team—especially if you’re a woman. At some point, you’re the only one who knows your body and knows when something is wrong.”
Andrea Frazier, 62

Photo credit: Nell Hoving
Heart disease survivor since 1989
Andréa Frazier had no reason to be suspicious of the headache she developed a few days after giving birth to her daughter in April 1989. But when the pain wouldn’t respond to over-the-counter medicine, she visited her ob/gyn and a neurologist. Neither seemed worried.
“By the time I was home from those appointments, I was in excruciating pain,” Frazier says. “It made childbirth feel like a papercut.” Frazier rushed to the ER, where tests revealed a slow bleed in her brain called a subarachnoid hemorrhage, a form of stroke. “At the time, I didn’t know I had hypertension that had spiked and contributed to the hemorrhage,” she says. “The pain I was feeling was from the blood causing swelling in my brain.”
Surgery was ruled out because the blood vessels leading to her brain had started to constrict and collapse. Instead, she had to remain flat on her back in intensive care and wait for the bleeding to stop. That nightmare lasted for almost two months. “I had planned to be home with my baby, nursing her and doing all kinds of new mother things, but I couldn’t even hold my daughter,” she says. “It was heartbreaking.”
When Frazier finally returned home, she knew she would need to be vigilant about treating the underlying cause of the hemorrhage. “I was put on blood pressure medication, which I take faithfully to this day,” she says. “I also began to treat my hypertension through diet, exercise and stress management.”
As she considered a second pregnancy six years later, Frazier made sure her heart was ready for another child. “My cardiovascular health was in very good shape, but toward the end I went into premature labor and ended up on bed rest again,” she recalls.
Today, Frazier encourages others to take an active role in their heart and brain health and is part of the American Heart Association’s initiative to improve access to fresh, healthy food in underserved communities in Philadelphia. Her two children have also taken her advice to heart.
“They both get their blood pressure checked regularly and exercise,” she says. “My son James runs track and my daughter Lauren ran the New York City Marathon. No couch potatoes in this family!”
For more information on ways you can Go Red this year, visit phillymag.com/gored.
This is a paid partnership between Go Red For Women and Philadelphia Magazine