This Philly Cancer Center Is Activating the Body’s Own Immune System to Target Tumors
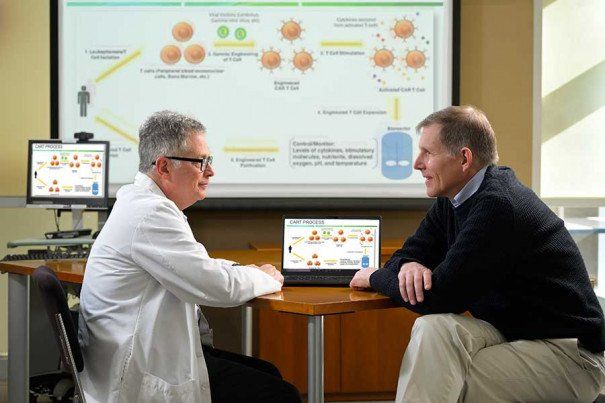
Courtesy of Fox Chase Cancer Center
In the early days of cancer treatment, patients with the same type of cancer tended to get the same type of treatment. Of course, the treatments worked better in some patients than others, and researchers began to find genetic explanations for those differences. This eventually led to a boom in “personalized cancer treatment,” where treatment is catered to both the patient’s genes and the cancer’s genes.
In recent years, the idea of personalized treatment took a big leap forward with a new treatment called CAR T-cell therapy that not only observed a patient’s genes to cater treatment, but altered the genes themselves to better attack the cancer. Now, researchers at Philadelphia’s Fox Chase Cancer Center are conducting a clinical study to expand that style of treatment, called adoptive cell therapy, to cancers that have not been receptive to it in the past.
“We’re paving the road for potentially a paradigm shift in the way that we offer therapy to patients,” says Dr. Anthony J. Olszanski, co-director of Fox Chase’s Melanoma and Skin Cancer Program and one of the physicians behind the ongoing study. “We’re beginning to develop therapies which are ultra-personal; in fact, they’re for a single patient.”
With CAR T-cell therapy, T cells, also called immune cells, are taken from the patient’s blood, and a gene is added that helps them identify the specific cancer cell antigens. They can then grow those modified cells into a type of cancer-fighting army and inject them back into the body. This gets at a central difficulty with treating cancer. Because cancer arises out of normal tissue, the immune system doesn’t attack it the way it does a foreign virus or bacteria. But by harvesting these cells, researchers can train them to see the cancer as foreign.
CAR T-cell therapies have been game-changing for some patients, including a fairly rare type of blood cancer called multiple myeloma, but they haven’t traditionally worked for solid cancer tumors, and diseases such as breast, colon, or lung cancer. The new treatment in trial at Fox Chase uses the same idea behind CAR T-cell therapy to harness a patient’s healthy T cells, but is modifying them to be able to identify the cancer present within solid tumors before returning the cells to the patient.
“What makes this revolutionary is that the cells themselves are the treatment,” says Dr. Martin J. Edelman, chair of Fox Chase’s Department of Hematology/Oncology.
The trial underway at Fox Chase focuses on non-small-cell lung cancer and is currently in phase two, meaning it’s been proven to be safe and they are now testing for efficacy in patients that have failed conventional treatment.
According to Dr. Henry Chi Hang Fung, the chair of Fox Chase’s Department of Bone Marrow Transplant and Cellular Therapies, non-small-cell lung cancer makes a good candidate because they have good data on the type of very specific T cells needed. Additionally, once it reaches the advanced stage, there are treatments to prolong life and quality of life, but no cure.
“This treatment would at least give the patient another option,” he says. “When they’re out of options, they’ll now have another one that has the potential to help them live long and have an excellent quality of life.”
Dr. Edelman says one of the things that makes this research so exciting is that it has the potential to be approved by the FDA and on the market within a few years.
“I would not be surprised if sometime within the next five years, one or more of these [adaptive cell therapy] approaches becomes approved and available in solid tumors, whether it’s for lung cancer or another cancer,” he says.
While adoptive cell therapy is on the cusp of approval for these cancers, there are some limitations that could keep it from becoming widespread, at least initially. The process of working with the cells outside of the body can take months and the uber-personalization of the process comes with a high price tag. It will also take a hospital with very robust infrastructure to perform the therapy.
For future patients, however, the impact of expanding adoptive cell therapy to solid tumors cannot be overstated.
“Immunotherapy is still new to the field of oncology,” Olszanski says. “And despite its relative youth, we have already seen vast benefits in patients. I really look forward to seeing what the next decade brings, because I think that I’m going to look back to today and think, ‘wow, we had so much we could learn, so much more to do.’ Every day brings a new recognition or realization for us.”
This is a paid partnership between Fox Chase Cancer Center and Philadelphia Magazine
