Delivering on DEI
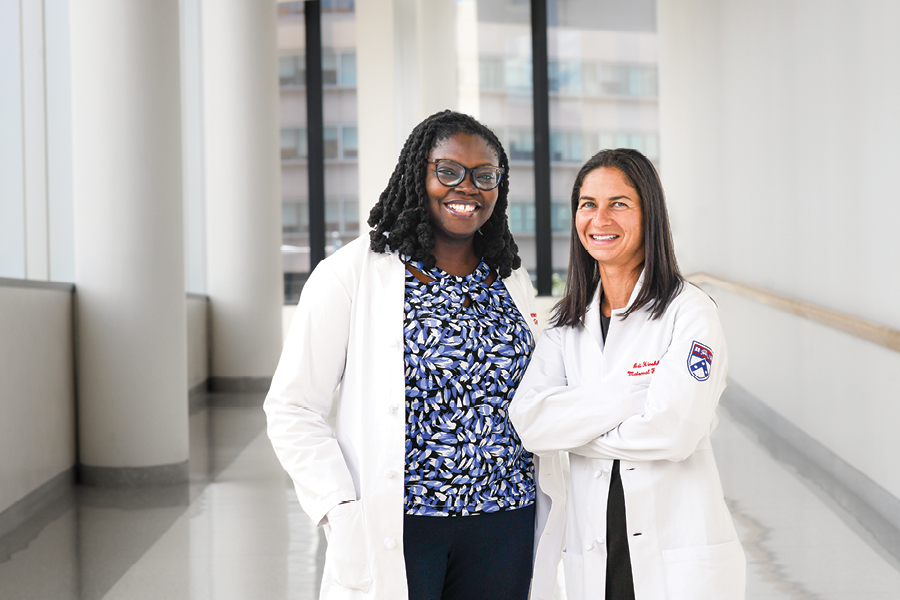
Penn Medicine is committed to removing barriers to care for women in the Greater Philadelphia area. Drs. Abike James and Adi Hirshberg discussed the ways they have worked with the health system to improve diversity, equity and inclusion (DEI) and how that has improved outcomes for patients.
In what ways have you supported DEI efforts at the Hospital of the University of Pennsylvania? Dr. Abike James: I have taken a multipronged approach to diversity, equity and inclusion, recognizing that it takes a village to see real change. In 2019, myself and colleague, Dr. Sarita Sonalkar, started our department’s health equity group, DISPEL (Dismantling Inequities, Systemic Problems, Elevate Lives). Our multidisciplinary task force focuses on education and quality improvement. Through examination of our own data and policies, we identified inequities within Penn Medicine and considered how we could improve.
›› How have these DEI efforts impacted outcomes for patients? AJ: I firmly believe that if all patients receive care in a diverse and inclusive environment that prioritizes health equity, health care for all will improve and disparities will be significantly reduced. For example, Penn Medicine established a system-wide goal to reduce maternal morbidity and mortality, and we worked toward this important goal as a team. In our first year, we were able to reduce maternal morbidity and mortality in Black women by 30% compared to the prior year. I have seen improvements in communication. I have witnessed providers (of all ethnicities) able to better communicate with patients and reassure them when they are scared. I have seen increased innovation and research aimed directly at addressing disparities. I have seen increased diversity in our teams leading to increased patient satisfaction. All these changes translate to improved outcomes for our patients.
›› Can you describe the HeartSafe Motherhood program? Dr. Adi Hirshberg: HeartSafe Motherhood is an innovative, patient-centered method of monitoring blood pressure for postpartum patients at risk of severe hypertension or preeclampsia after delivery. Knowing that blood pressure can increase after patients are discharged and that the risk of hypertension-related morbidity and mortality is high in the first 10 days after delivery, the program provides patients with blood pressure monitors and prompts them to check their blood pressure twice a day via text messaging. Patients can then text back their readings and receive feedback about whether it is high or not. If the blood pressure is very high, a provider will contact them to help determine next steps. The goal is to catch rising blood pressure and treat it before it results in complications.
›› How does the program help to eliminate some of the racial disparities of postpartum care? AH: Because patients are given blood pressure cuffs and we use low-tech text messaging to communicate from any location, we are able to obtain blood pressure readings from patients regardless of insurance, wireless access and other barriers that may affect in-person care for one group over another, like childcare or transportation. Without this program, about 70% of white patients attended in-person blood pressure checks compared to 33% of black patients. HeartSafe Motherhood has helped eliminate many racial disparities, with 90% of patients now engaging in blood pressure monitoring, regardless of race.
This is a paid partnership between Penn Medicine and Philadelphia Magazine

