This Philly Doctor Invented a Way to Dissolve One of the Most Dangerous Types of Blood Clots
For blood clots that cause heart attack and stroke, immediate treatment through surgical removal or dissolution with blood thinners can be life-saving. But what happens when a blood clot that causes blockage to the blood flow in the lungs grows too large to safely remove through either method? Until recently, there was no clear solution—and the problem occurs more often than you might think.
Pulmonary embolism is the third most deadly cardiovascular condition, along with a related clotting condition called Deep Vein Thrombosis (DVT), after heart attack and stroke. Both conditions involve blood clots and affect 900,000 people and cause approximately 100,000 deaths annually in the U.S. alone.
But unlike the clots that are usually responsible for heart attacks and strokes, clots in patients with DVT and PE are normally far too large to be effectively and safely dissolved using medication or minimally invasive surgery. No perfect, widespread solution for this deadly condition exists.
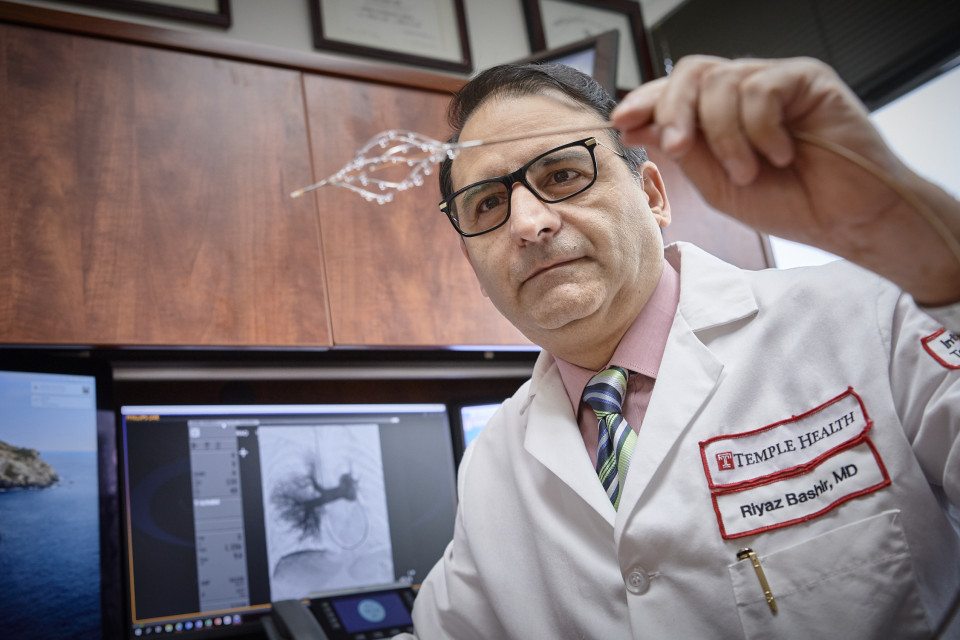
And yet there’s hope in Philly. A Temple Health cardiologist, Dr. Riyaz Bashir, has invented a groundbreaking new treatment for blood clots in large veins, and for the treatment of DVT and PE, one that uses the body’s own blood to help dissolve clots with greater success rates and less medication. So far, it’s been used on less than 200 patients. But as it expands globally, the treatment could change the way physicians treat blood clots.
The best treatment for blood clots is already inside your body.
As a cardiologist, Bashir was dissatisfied with current treatment options for DVT and PE, which primarily consisted of medication or suboptimal removal of blood clots. When you try to remove a massive clot with a catheter, you risk sending debris from the clot deeper into the patient’s veins and arteries. However, if you try to dissolve the clot using medication, you risk potentially deadly side effects, including internal bleeding into the major organs, even the brain.
But Bashir, after years of observing clotting behavior in the body, had a critical insight.
“The patient’s own blood has a lot of clot-dissolving chemicals in it that can rapidly dissolve the clot. The most potent clot dissolving medicine in the body are enzymes in its own blood,” Bashir says. While clots are composed of a material called fibrin that resist the blood’s natural tendency to break things down, once the fibrin comes into contact with a small amount of a clot-dissolving medicine called a thrombolytic, it activates the enzymes in the blood to break down the blood clot.
“Once you combine them [medicine and the patient’s blood], there is a dramatic synergistic effect between the two,” Bashir says.
So Bashir set about designing a catheter that would send a small amount of medicine directly into the clot while opening a channel through it to allow blood to flow in—enabling the body to heal itself with minimal risk of side effects.
The result was surprisingly intuitive. The BASHIR™ Endovascular Catheter has a collapsible basket at its tip that can be expanded once inside a clot. This fissures into the clot, opening it up to allow blood to pass through. The physician can then deliver clot dissolving medicine from each limb of the basket. Thanks to the opening action of the basket and the medicine, blood goes to work dissolving the clot on its own.
“It brings the patient’s own blood into the clot,” Bashir says. “It then saturates the clot with the clot dissolving medicine, and let’s the blood dissolve the clot.”
Thanks to a doctor’s insight, blood clots once thought untreatable can now be safely dissolved.
The arrival of a catheter with the ability to restore blood flow through a clot instantly has important implications for the future of treatment. Bashir’s approach allows him to tackle the numerous challenges traditionally posed by blood clots.
Bashir’s first concern when working on a patient with a blood clot is restoring blood flow to critical areas as quickly as possible. His catheter makes that possible.
“A lot of these patients can get very, very sick very quickly—within minutes,” Bashir says. Upon the basket’s expansion, some amount of blood flow Is immediately restored, limiting potential damage from lack of oxygen. “The ability to open up a basket and have blood flow restored can be the difference between life and death for some of these patients.”
Bashir then wants to dissolve as much of the clot as possible. At the heart of Bashir’s design is the simple fact that other catheters, which are also placed inside of blood vessels, aren’t big enough to affect the bulk of the clot without a dangerous dose of medicine.
“One of the main inspirations for the development of this catheter was these blood vessels. Their diameter is 25 to 30 millimeters, and we were using devices that were made for 5 millimeter vessels,” Bashir says. “No wonder they weren’t doing a good job! So what I tried to develop was a device that can be used in larger vessels.”
The device’s ability to expand in size and break through these large clots allows a much larger surface area of the clot to get exposed to the clot dissolving medicine. Investigational device studies, including the ongoing RESCUE trial, show that the catheter reduces the dose of medicine needed by a third or more, and reduces treatment time from 12 hours to five hours, showing greater overall success rates in dissolving clots. That lowers long term risks of thromboembolic disease, lung hypertension and other symptoms, in addition to increasing survival rates.
The small change could impact thousands of lives.
Its efficiency was critical for Marc Gilliard, a 55-year-old Philadelphia resident and one of Bashir’s early patients.
This past February, Gilliard’s legs doubled in size. He couldn’t stand, and the chest pain made him believe he was having a heart attack.
Gilliard was taken by ambulance to the closest hospital available, which fortunately happened to be Temple. DVT clotting ran throughout his legs. It was so extensive, he had to remain in his hospital bed with catheters in his veins for two days. At one point, he told his doctors he was afraid he was about to die.
But thanks to the treatment by the BASHIR™ catheters, his physicians were able to clear all of the clots in his abdomen’s main vein and veins of both legs without the use of drugs that could have further damaged his kidneys. Two weeks later, he was able to walk again.
“I was blessed, because I had a good team, I had good doctors,” he says. His doctors told him if he hadn’t received appropriate treatment when he did, he would’ve died. “I believe God blessed me to go there because they have it all in place already.”
Bashir hopes that stories of recovery like Gilliard’s will soon be standard. He thinks use for DVT and PE will grow. The device is currently in clinical trial for pulmonary embolism, which affects half a million Americans each year. The journey he started as a cardiologist looking for a better way to treat his patients is nearing its end.
“I always think of cases I have treated in the past where I think, my goodness, I wish we had this device at the time,” Bashir says. “There are a lot of patients that are suffering because they didn’t have treatment like this.”
Editor’s Note: Dr. Bashir is a co-founder and has equity interest in Thrombolex, Inc. a medical device company developing interventional catheter-based therapies for the rapid and effective treatment of acute venous thromboembolic disorders. Temple University also holds a financial interest in Thrombolex, Inc., pursuant to the license granted to Thrombolex for the University’s interest in the patent filed for the experimental catheter device developed by Dr. Bashir and Nicholas Green.
Temple licensed Dr. Bashir’s patent to Thrombolex, Inc., a Pennsylvania medical device company, so they could develop the actual product, named the BASHIR™ Endovascular Catheter and secure the FDA clearances to market and commercialize the initial product and its subsequent versions.
This is a paid partnership between Temple Health and Philadelphia Magazine
