The $850K, Philly-Developed Blindness Treatment That Could Be the Gateway to Curing Big Disease
Spark Therapeutics's new drug may be worth every cent.

Spark Therapeutics president and head of R&D Kathy High. Courtesy photo.
Last month, the U.S. Food and Drug Administration (FDA) announced its approval of Spark Therapeutics’ Luxturna, a one-time treatment for adults and children with a rare form of inherited vision loss that can lead to blindness. And on Wednesday, the company announced that the drug will cost $850,000 per patient — below the $1 million price tag analysts expected.
The FDA’s approval is historic since Luxturna is the first directly administered gene therapy approved in the U.S. that targets genetic disease. After decades of gradual successes — and also big failures in the field — the FDA says we’re at a turning point. At the announcement, Commissioner Scott Gottlieb said that gene therapy will likely become a “mainstay in treating, and maybe curing, many of our most devastating and intractable illnesses.”
BizPhilly sat down with Kathy High, Spark Therapeutics’ president and head of R&D to learn more about the company’s demanding path to FDA approval. High explains why gene therapy has been so challenging and why Luxturna’s approval is such a big deal. She also addresses the price controversy surrounding gene therapy and those naysayers who argue the therapies aren’t worth pursuing. Plus, because two of the three gene therapies approved in the U.S. are out of Philadelphia, High explains what it all means for the city.
BizPhilly: It was a groundbreaking moment last month when the FDA approved Spark’s Luxturna, a gene therapy for a rare form of blindness, the first such treatment cleared in the U.S. for an inherited disease. Can you talk about the significance of the FDA approval?
High: From the early stages of the Human Genome Project everyone hoped that eventually we would be able to use genes as medicine, particularly for genetic disease. The idea is that if a person is born with a genetic disease we would have the option to replace a defective gene with a normal copy. Of course, as you know, it has taken a while to really introduce that into practice. But that is what we’ve been working on all this time.
Gene therapy is one of those concepts that is deceptively simple. It has proved challenging to put into practice, but after a long road, we are finally here. At the press conference, FDA commissioner Scott Gottlieb said, “I believe that gene therapy may hold the key to treating a number of devastating diseases for which we now lack treatment.” And that is exactly why this is important. The licensing of Luxturna was the culmination of many years of effort to develop what is the first licensed approved gene therapy for genetic disease in the U.S. The two earlier approvals this year (Novartis’ Kymriah and Gilead Sciences’ Yescarta) were for cancer, which is important, but what we have been working on at Spark for all these years is gene therapy for genetic disease. This is obviously an exciting time for us. I started working on this program in 2005.
BizPhilly: Wow, it’s been over a decade. Can you say more about the history of the program in Philadelphia?
High: Yes. The Luxturna program was launched in 2005 and the way this came about is wrapped up in gene therapy’s embattled history. The first trials of gene therapy for genetic disease began in 1990, and for the first decade, many trials took place for cystic fibrosis, hemophilia and other diseases. Generally, they looked safe but they were not compellingly effective. Then in 1999 there was a high-profile adverse event in a Philadelphia gene therapy trial and a few years after that, children who received another type of gene therapy in Paris unfortunately developed leukemia. After those adverse events, support for the gene therapy field from investors and from tech and pharmaceutical companies collapsed. So most of the work moved back to academic medical centers.
At the time I had been collaborating with a tech company in northern California, but they also decided to get out of gene therapy. I decided to go to the CEO of Philadelphia’s children’s hospital to ask him if I could continue my work in his hospital. He came back and said he would support me because he believed that gene therapy and the burden of genetic disease falls very heavily on children’s hospitals. Nationwide, something like 50 percent of the admissions to children’s hospitals are for genetic diseases like sickle cell, cystic fibrosis, muscular dystrophy or hemophilia. He decided to support me, but his one request was that I work on other genetic diseases. All of my work up until that time had been on hemophilia. But I told him that would be no problem because I was already familiar with the work that Jean Bennett was doing at Penn for the rare form of congenital blindness.
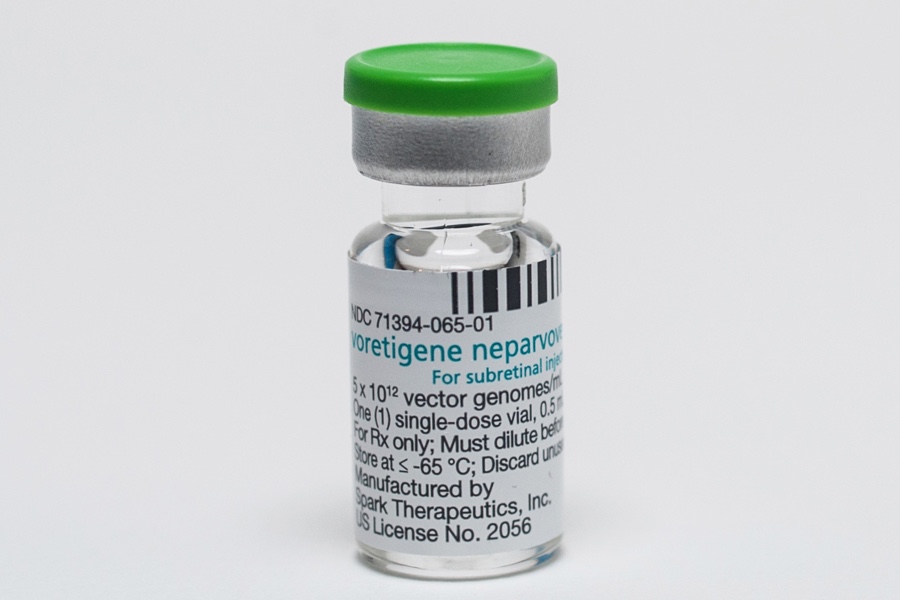
Product vial. Courtesy photo.
BizPhilly: How did you get things going once you got CHOP on board?
High: In 2005, Jean Bennett agreed to work with us. We spent the next two years trying to do all the studies we needed to get set up to do a clinical trial. And in the fall of 2007 we started the trial at CHOP. Everything went fine, and at the end of the work in 2009, we approached the FDA to ask what we would need to do to take this to a trial for licensing. They first told us we’d have to prove that the treatment was safe to inject in our patients’ other eye. So we did another trial with all of the people who had been in our first trial and brought them back in and injected their other eye. When that was through, in the summer of 2011, the FDA held what is called an advisory committee meeting to give us advice over the next year on what our Phase 3, or pivotal trial, should look like.
BizPhilly: And according to the FDA, Phase 3 was crucial in proving Luxturna’s efficacy. Why was this step so important?
High: It was so important because the FDA wanted us to find a new endpoint since this was a class of diseases that had never previously had a treatment. At that point there wasn’t a clear idea on how to measure a response or progress. And I know that might sound non-obvious to readers who would say that the difference should be whether participants are able to see or not see following treatment. But it doesn’t necessarily work that way because vision is made up of many different components. The main defect with this kind of blindness is a person’s ability to detect light. We had to come up with a new way to measure the effect of your ability to sense light on what you can do. So in other words, there is already a test for measuring whether or not people can sense light but the FDA wanted to know how that affects a person in their daily life. This was the novel endpoint we had to come up with. We tested participants’ ability to navigate twelve different mazes or obstacle courses that we set up at different light levels. And it had to be designed in such a way that a skeptic would be convinced that the treatment made a difference for people. 93 percent of all participants were able to show improvement on the test and 72 percent got to the point where they could navigate the course at the lowest light level.
We, and also the FDA, are very proud of this work because it illustrates a hurdle for teams that are trying to use gene therapy to attack diseases that have never had a treatment before. We know this will not be the last time this hurdle is encountered.
BizPhilly: What’s your response to people who say it’s not worth it to work on this treatment since the disease affects just 1,000 to 2,000 people?
High: That is a very important question. One reason I thought it was important to do this disease even though it does not affect many people is that it had a very clear proof of concept in a large animal model. It turns out that you can make a mouse model of almost any disease and then you can cure that model. But, unfortunately, most of the things that have worked to cure mice don’t really work in people. If, on the other hand, you can cure a dog, you are much closer to the real thing. I thought about this is when I sat and watched the first decade of clinical gene therapy people try to tackle big diseases like cystic fibrosis and muscular dystrophy. They were such big diseases and the technology was not good enough yet so all of those things failed. I said, “let’s do something that will work.” I thought that if we can show that we can cure it in a dog then we have a much better shot. So while it may be true that just 1,000 to 2,000 are affected, the art of gene therapy at this point in the field is to choose the things that work. It doesn’t matter how important the disease is. If it doesn’t work, too bad — it didn’t really help anybody.
Plus, there are over 250 genes involved in vision so this really is a gateway. Does it mean that we can develop a cure for every single one of these genes? No. It doesn’t mean that. But I feel quite sure that the next clinical development program for inherited retinal disease will not take ten years because along the way we worked out the solutions to a number of problems. When we come to them again, we won’t have to solve them.

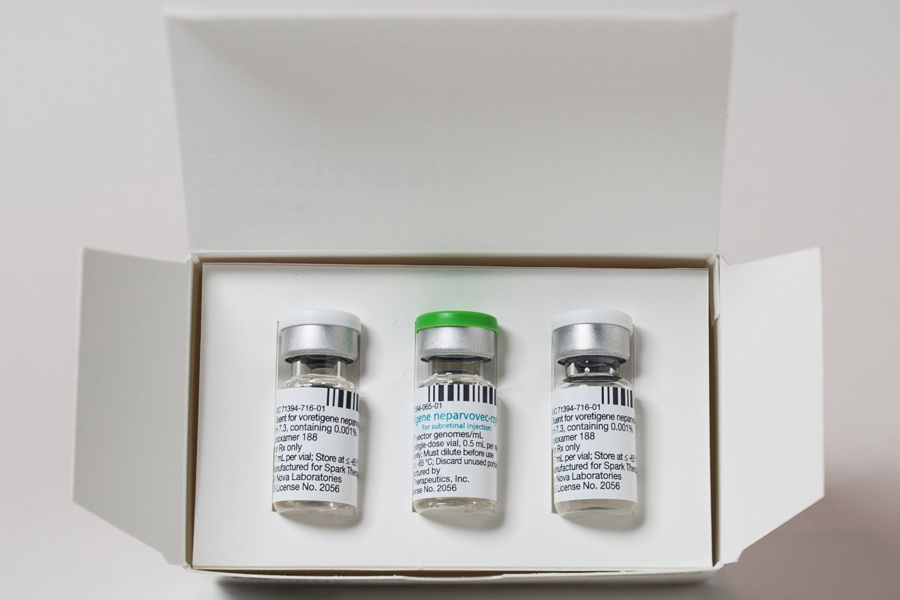
Product vials. Courtesy photo.
BizPhilly: What would you say this gateway means for Philadelphia?
High: Well, let me say this first: I am really biased because I have Philadelphia pride. To me, it is very important that this is work that started here. This is work that the Children’s Hospital of Philadelphia and Penn supported when other people did not, and when other people believed that this would not work. It was also really important that we formed Spark. There are a few areas in the U.S. that have a great wealth of technology companies — San Francisco, San Diego, Boston — but it was very important to me that we keep our research in Philadelphia. We did all of the preliminary work here. This should be something that benefits our city. I am very proud of the fact that we have built up our technology right here in West Philadelphia. We have over 300 employees at Spark right now. We are a premier gene therapy company and nobody would dispute that. We built that here in Philadelphia.
BizPhilly: And what does the FDA approval mean for people with inherited retinal dystrophies?
High: I have to say that the retinal dystrophy community has been incredibly helpful and incredibly inspiring for our work. I’m most impressed by the fact that some of the strongest support we got on the day of the FDA advisory committee meeting back in October came from parents of children who had other inherited retinal dystrophies. They did not even have what Luxturna is for, but they spent their time and resources trying to help explain to the advisory committee exactly what it means to have a child with visual impairment, exactly what it means to try and educate a child who may have never seen the things you are trying to teach about. They did that because they realize this is the gateway.
What it means for these people is best illustrated through the testimonies of the people who have gone through the clinical trial. One 24-year-old woman who is now a research assistant at the VA hospital in Los Angeles talked about how her vision started deteriorating when she was in college. She was a math and biostatistics major and even though she used a lot of visual aids to try and help her get through her work, her vision deteriorated semester by semester to the point where she wasn’t sure she would be able to move forward with what she wanted to do in life. But she enrolled in our study and her vision improved to the point where she could finish college, get a graduate degree and now work at the hospital.
BizPhilly: A heated discussion around gene therapies right now is cost. They’re proving to be some of the most expensive drugs ever. What are your thoughts on the price debate?
High: Firstly, we have not worked on this for the last 12 years to set up a situation where people who need it can’t get it. I do not want that to happen. Spark has spent a considerable effort trying to make sure that any patient that could benefit from it will have access to it.
Secondly, I am sure you understand we spent at least 12 years (not counting all the work that Dr. Bennett did before that) trying to bring this to where we are now. It will be important in my view for Spark to be able to sustain itself so that we can develop products for other inherited retinal dystrophies. We will not have the advantage that most medicines have of being able to charge every time you take a pill. This is designed as a one-time treatment. Our current pharmaceutical reimbursement system is basically set up to favor treatments that are given over and over again. Ideally, it should be set up to reward treatments that you only have to do once, which make everybody’s life easier. So, I would say that we are in the new era of what drug development can do, but we currently exist in the midst of a payment system that is really designed for the previous era. So we will all have to work together to develop something that appropriately accounts for the huge cost that went into developing this and the fact that it will not be something people take year in and year out for the rest of their lives.
So do I know the answer about the best way to do that? No. I don’t. But as I said at the outset, we didn’t do all of this work so that the people who need it can’t get access to it.
Courtesy photo.
BizPhilly: What is next for Spark Therapeutics now as we move into the New Year? How do you pivot after getting such an approval?
High: That is a very important question because I’d like to point out that there were two products previously licensed in Europe for gene therapy for genetic disease. The first was for a rare lipid disorder. The people who developed the treatment and had it licensed to them announced in the fall that they are not going to renew the license because in the five years since receiving it, they only sold one dose. That company tried not once, not twice, but three times to get the product licensed. But by the time they got it, they had laid off a lot of the company. They weren’t really able to make a concerted commercialization effort. And for the other gene therapy licensed in Europe, which was for a very rare form of immune deficiency disorder, they haven’t sold very much either since there’s another treatment for the disease.
At Spark, we would like for the launch of this product to be a success. We would like for it to reach people who need it and for their treatment to be a success. We have taken a number of steps in that regard. We’ve spent a good time upfront talking with insurers. We have a group of employees who will help patients gain access. We have confined the initial administration of the product to a few centers of excellence in the U.S. where there is all of the expertise needed to diagnose the patients with the disease and to do a pristine surgical procedure to administer the product. This is one way we differ from Novartis’ Kymriah. With that treatment the cells are taken out of the patient, destroyed in the laboratory and returned to the patient. For this, the dug comes in a vial and the pharmacy preps it and the surgeon gives it in the operating room.
BizPhilly: As gene therapy continues to get some major wins, what are you most looking forward to?
High: In the field, I’m really excited about another company’s product. It is for spinal muscular atrophy, a rare disease that affects infants. The company, AveXis, is seeing some wonderful results. I think that they could see approval in the next year or two. I’m also excited about the work that we and others are doing in hemophilia. I have worked on that for a long time but to me what we have now are transformative results. Instead of taking three intravenous injections a week for the rest of your life, these people are getting a single injection. And in our first hemophilia trial, which is partnered with Pfizer, these people are two years old now. They took one injection and now that’s all they have had. That is very exciting to me. We have a clinical program for two different forms of hemophilia and a program for another inherited retinal disease. We have a lot of things in our pipeline.
I am just delighted that after a very long road we reached approval. I am particularly grateful to not only the pioneers here at Spark and the people we worked with on our clinical trial, but I am especially grateful to the patients who took a big risk in signing up for the trial because nobody could guarantee them anything. Of course, without their participation there will never be new treatments. In many ways, they are the real heroes.